What is atrial fibrillation?
Atrial fibrillation is the most common cardiac arrhythmia ..
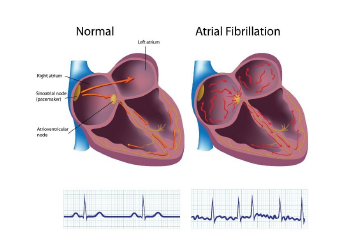
It is generated in the atria and causes the loss of regularity of the heart rhythm.
The atria are activated at a frequency of 400/600 per minute , a great electrical acceleration that no longer produces any contraction: inside them the blood tends to stagnate and coagulate.
The ventricles fire irregularly and often at an accelerated rate, reducing the efficiency of their hydraulic pumping action, which pushes blood through the circulatory system.
The consequences of this arrhythmia are therefore the perception by the patient of an accelerated and irregular heartbeat , a reduction in the efficiency of the cardiovascular system of varying degrees up to cardiac failure and the risk of thromboembolism and cerebral stroke.
How is the diagnosis made?
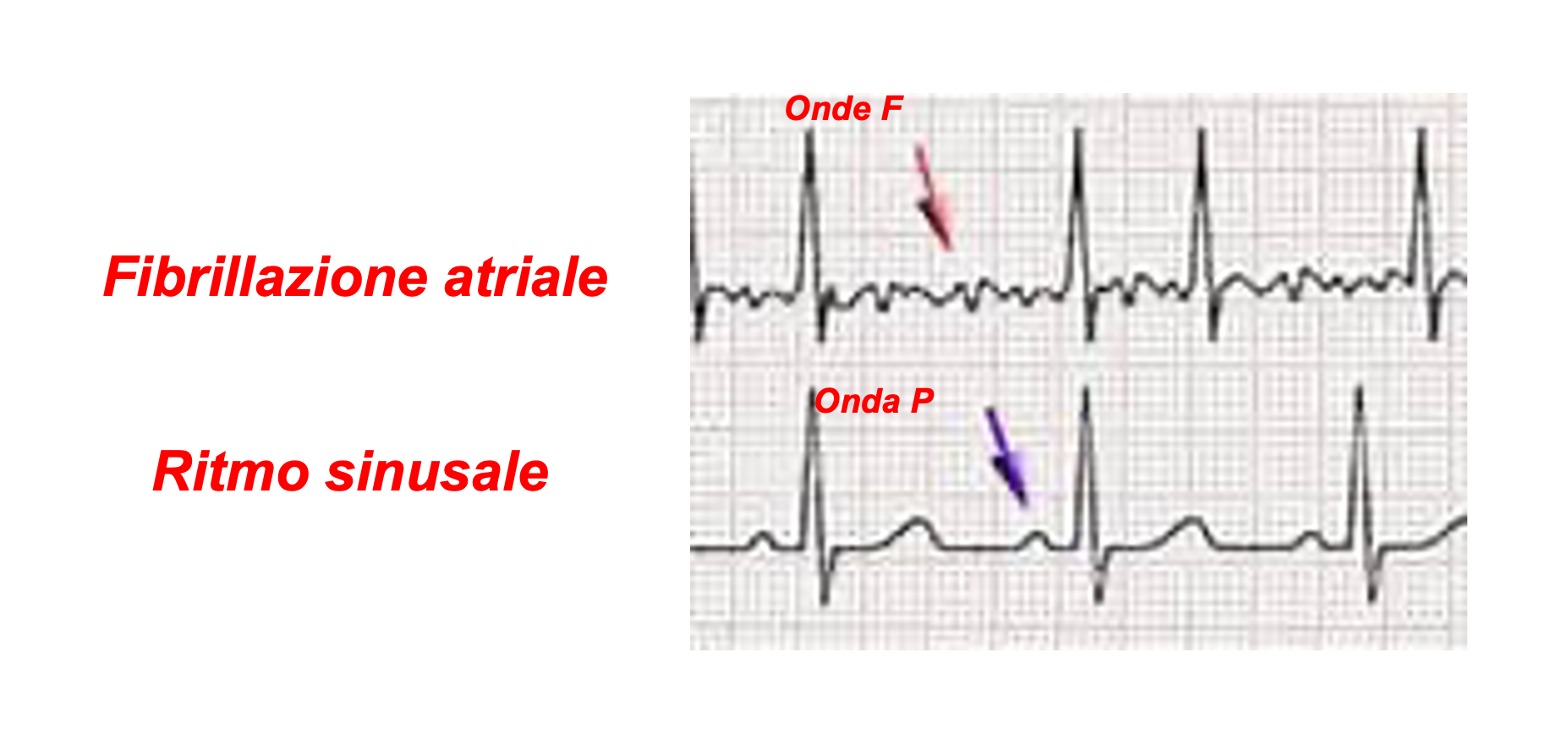
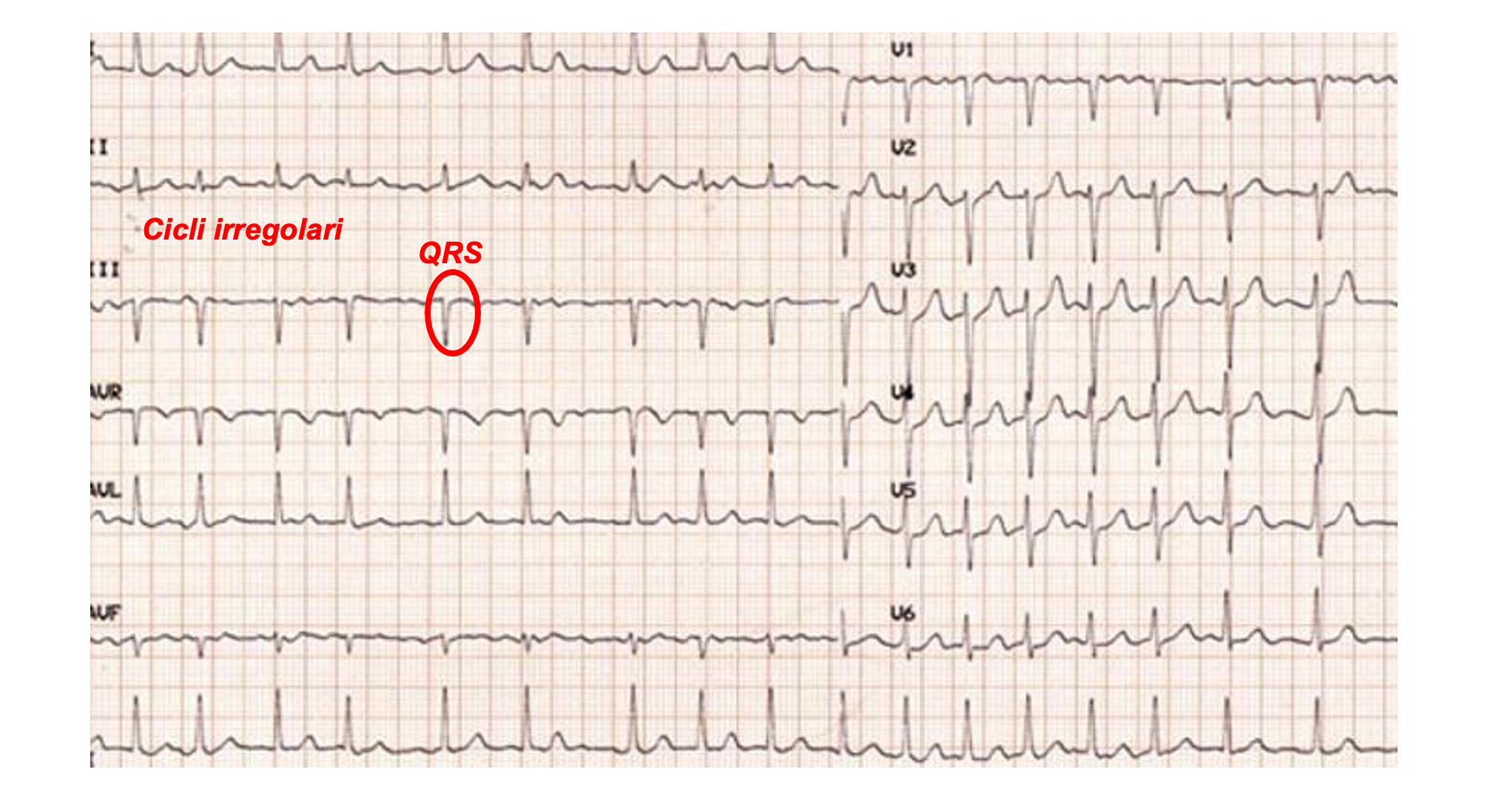
The diagnosis of atrial fibrillation is made with the electrocardiogram: during atrial fibrillation the rhythmic P waves that characterise sinus rhythm disappear and are replaced by irregular F waves with a very high frequency (400-600 bpm) .
Cardiac cycles characterized by QRS complexes become rapid and irregular.
To make a diagnosis, it is necessary to record the electrocardiogram during the occurrence of atrial fibrillation.
Since this can be intermittent, it is often necessary to use long-term electrocardiographic recording systems that can detect the arrhythmia when it occurs. In these cases, we speak of holters lasting from 24 hours to 30 days.
There are also subcutaneous implantable devices capable of recording the electrocardiographic tracing in the event of the onset of arrhythmia, even if asymptomatic, and transmitting it via the Internet to the reference cardiology center.
Today, there are electrocardiographic recording devices inserted into smart watches, small external recorders that work in a similar way.

How common is atrial fibrillation?
In Italy, according to ISS data, atrial fibrillation affects approximately 1-2% of the population: data in line with those of the Western world. Its incidence increases with age .
In Italy, 8.1% of people over 65 suffer from atrial fibrillation, for a total of approximately one million people.
Eurostat demographic estimates predict a doubling of prevalence by 2060 to approximately two million cases.
It is therefore an extremely widespread disease, one of the most frequent causes of access to the emergency room and with a very high economic and health impact destined to increase further with the progressive increase in the elderly population.
Who gets hit?
Although this disorder can occur in subjects without heart disease or other pathological conditions (isolated atrial fibrillation), it is often associated with cardiac or extracardiac pathological situations that facilitate its onset by causing an alteration of the atrial electrical substrate.
All heart diseases of valvular, ischemic, degenerative, inflammatory, genetic and idiopathic origin can constitute a risk factor for the onset of atrial fibrillation.
Furthermore , advanced age, obesity, diabetes, hypertension, lung disease, sleep apnea, hyperthyroidism are significantly associated with a higher risk of onset.


How does it evolve and how is it classified?
Atrial fibrillation has a worsening trend over time.
It almost always begins intermittently: the episodes are initially rare and short-lived. We speak of paroxysmal atrial fibrillation when their duration is less than a week. We are in a situation in which the disease of the atria is still mild, their size is still almost normal and the fibrosis of the tissue is absent or mild.
As time passes, the disease progresses, the atria dilate, undergo fibrotic degeneration and the duration of the episodes becomes increasingly longer: when it is between a week and 12 months, it is called persistent atrial fibrillation . If it goes beyond 12 months, it is defined as long-lasting persistent atrial fibrillation .
Obviously, the possibilities of effectively treating this pathology depend on the degree of progression of the disease. A long-lasting form implies an advanced atrial disease and at a certain point the various therapies implemented will no longer give any results. The doctor will therefore be forced to give up interrupting the arrhythmia. In this case we speak of permanent or chronic atrial fibrillation .
Each episode of fibrillation produces a worsening of the atrial electrical situation; fibrillation generates fibrillation in a vicious circle that, if not interrupted in time, makes the treatments less and less effective.
What are the consequences of atrial fibrillation?
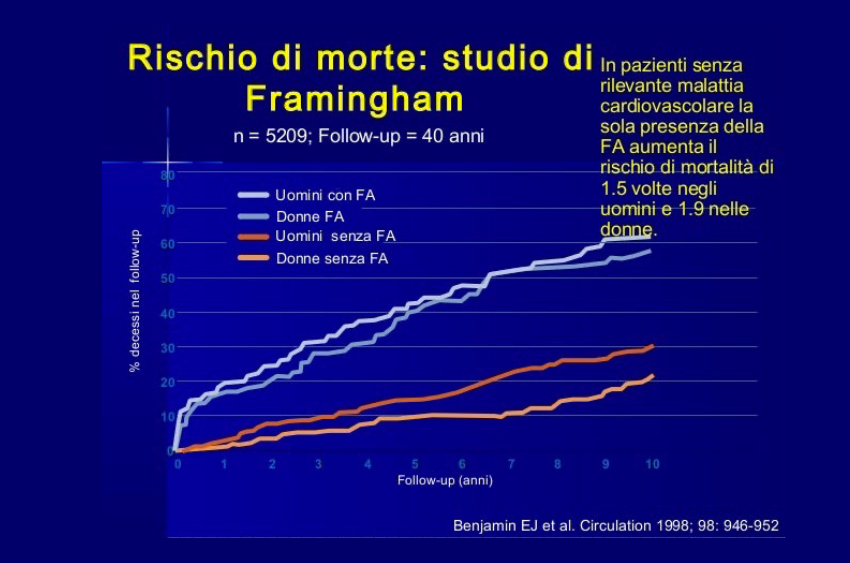
Patients with atrial fibrillation tend to have shorter, less healthy lives compared to those without the condition.
Mortality data from several studies have shown an increased risk of death of between 1.5% and 2% in subjects with atrial fibrillation compared to controls. Ten years after the start of the Frahmingam study, 60.1% of the affected patients had died, compared to 30% of the unaffected subjects.
The risk of sudden death also appears to be increased in affected subjects with a risk of approximately 1.8% compared to unaffected subjects.
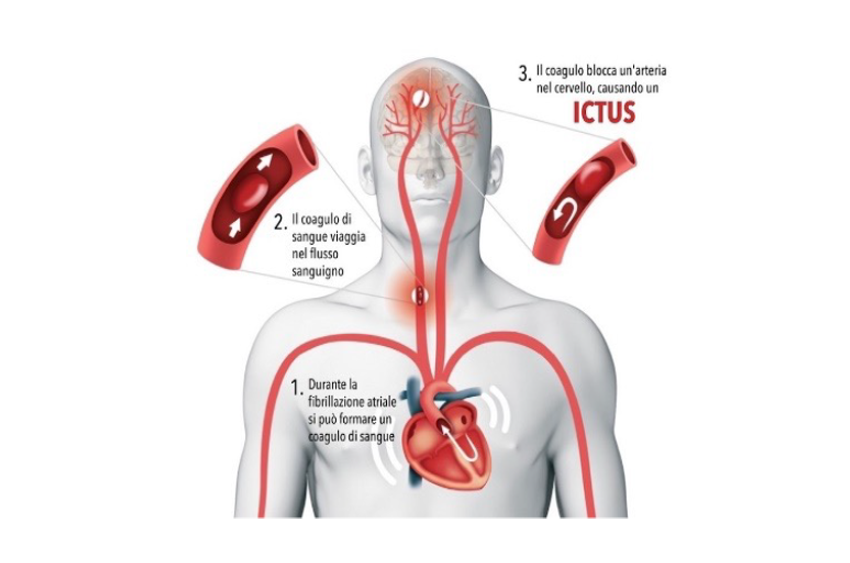
Mechanical paralysis of the atrium promotes stagnation and coagulation of the blood inside it, which leads to the risk of thromboembolic events, the most feared of which is cerebral stroke .
The risk of stroke varies from 0.7% to 23% depending on age and the presence of concomitant risk factors.
For the prevention of cerebral stroke, adequate anticoagulant therapy is necessary, which has demonstrated a good capacity for preventing thromboembolic phenomena and an absolute reduction in the risk of death of 1.6%.
Even in the absence of a stroke, patients with atrial fibrillation may experience a decline in cognitive functions of varying degrees, leading to dementia. At least one third of patients with atrial fibrillation have microembolic lesions on brain MRI. The risk of dementia is higher in patients with onset of atrial fibrillation under the age of 67: at a young age, cerebral blood flow is more altered during atrial fibrillation and this can cause cognitive deterioration in the long term.
There is a very close link between atrial fibrillation and heart failure. Irregular and accelerated cardiac activity, with loss of atrial contractile function, makes the heart function less efficient. This situation can cause heart failure de novo or significantly worsen a pre-existing condition.
In addition to its impact on mortality and potentially serious complications, atrial fibrillation causes a deterioration in quality of life. The sudden onset of heart palpitations often prevents the patient from carrying out regular daily activities. In many cases, it is necessary to visit the emergency room for urgent, specific medical care.
In longer-lasting forms, even without reaching full-blown heart failure, it can cause a reduction in the patient's physical performance, who will therefore suffer a more or less marked functional limitation.
Reduced cognitive functions also alter the intellectual performance of affected subjects.

Overall, therefore, atrial fibrillation has a negative impact on the quality and expectancy of total and healthy life.