What is Wolf Parkinson White Syndrome?
Wolff-Parkinson-White syndrome (WPW) is a congenital arrhythmic disease characterized by the presence of one or more accessory anomalous atrioventricular bundles, which can give rise to arrhythmic episodes. The average prevalence is estimated at 1 in 450 people.
WPW Syndrome affects mostly males (70% of cases) at a young age. Under normal conditions, the electrical impulse originates in the atria and is conducted to the ventricles through a single point of contact: the atrioventricular node (fig. 1).
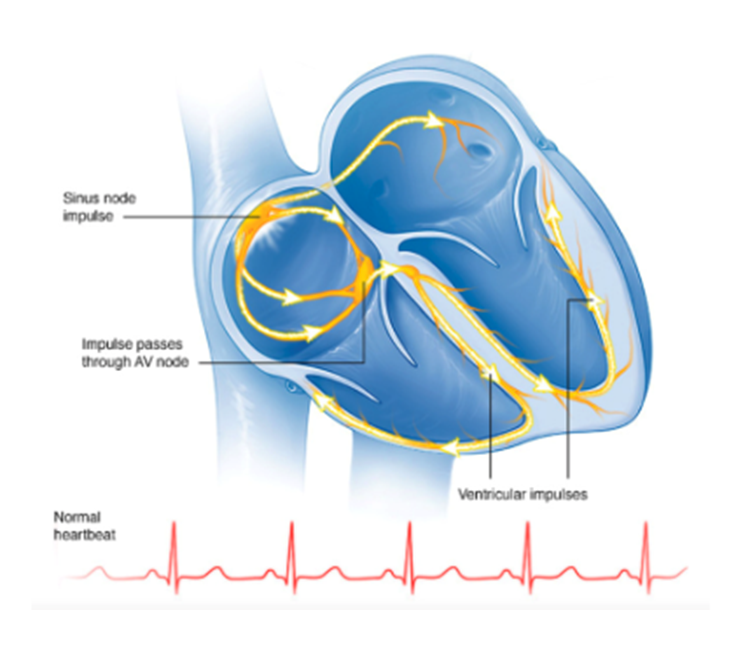
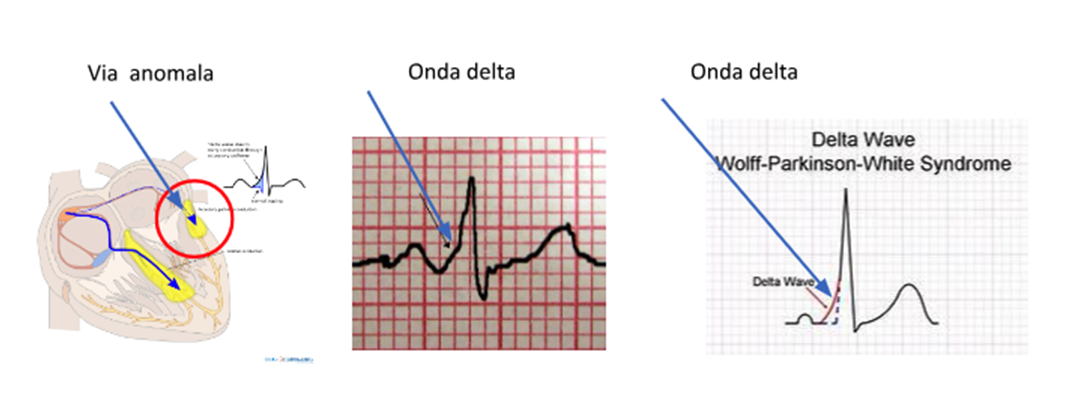
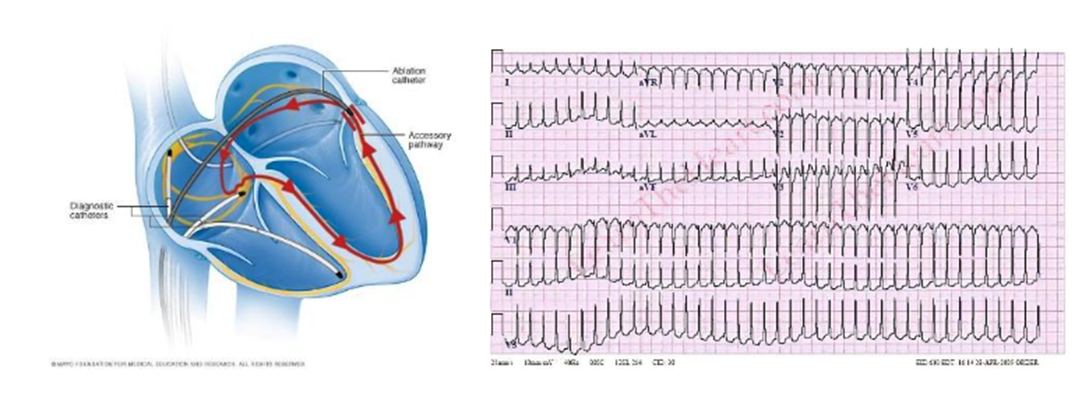
In WPW syndrome, there is a second electrical contact point between the atria and ventricles called accessory bundle or anomalous pathway. The electrical activation of the ventricles therefore occurs in parallel between the normal pathway and the accessory pathway, determining the classic electrocardiographic appearance called ventricular pre-excitation with the presence of the delta wave (fig 2).
What are the consequences of WPW Syndrome?
The physiological conduction pathway, in the atrioventricular node, is able to perform a filter function on the impulses that reach the ventricles from the atrium. In the case of arrhythmias that greatly increase the atrial frequency, such as atrial fibrillation, the frequency transmitted to the ventricles is limited by the atrioventricular node to allow the heart to perform a pumping function that would be impossible at excessively high frequencies. The accessory pathway responsible for WPW syndrome, however, does not have this safety filter function and can transmit high frequencies to the ventricles that can lead to cardiac arrest. For this reason, WPW syndrome can be burdened by an increased risk of sudden death. (Fig. 3)
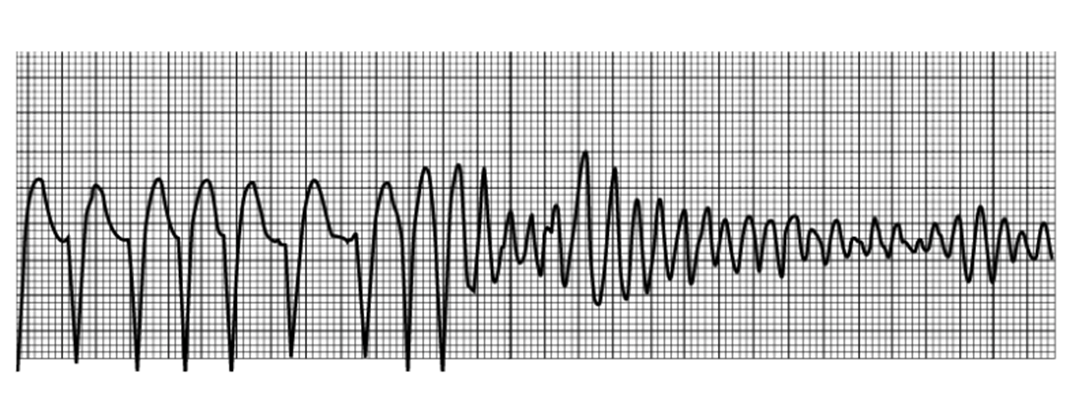
Furthermore, the anomalous pathway may constitute a branch of an electrical short circuit that underlies a paroxysmal supraventricular tachycardia.
In this case, the electrical impulse travels regularly along the conduction pathways from the atria to all the ventricles; at this point, instead of switching off to make room for the activation of the next heartbeat, it rises upwards through the anomalous pathway, returns to the atria to descend again to the ventricles through the normal pathways, giving rise to a continuous cycle that activates the heart at a very high frequency, giving rise to paroxysmal tachycardia . (Fig 4)
How is WPW Syndrome diagnosed?
The diagnosis is made with the electrocardiogram based on the presence of a characteristic wave called the Delta wave (fig. 2).
However, sometimes the anomalous pathway may not give rise to a delta wave and the basic electrocardiogram may be normal. In these cases, the anomalous pathway lights up only when a paroxysmal tachycardia is triggered and the pathway conducts the impulse backwards. In these cases, the presence of an anomalous pathway may be suspected on the basis of some aspects of the electrocardiogram during the tachycardia and the clinical characteristics of the patient, in particular the onset in childhood or adolescence.
When the delta wave is not present, an electrophysiological study is necessary to make a definitive diagnosis .
How is risk assessed in patients with WPW syndrome?
The worst risk to which patients with this syndrome may be exposed is cardiac arrest and sudden death. Fortunately, this is a rare event that occurs in approximately one case out of a thousand affected patients. The danger of the pathway depends on its ability to conduct the cardiac electrical impulse. In case of high conduction capacity, the pathway is considered high risk, while if the pathway has poor conduction capacity, it is considered low risk.
This parameter is measured through electrophysiological study: the test is generally recommended to patients who complain of symptoms such as palpitations or fainting. Asymptomatic patients are generally considered low risk and are subjected to electrophysiological study only in case of need for competitive sports fitness or for carrying out professions with particular risk and responsibility towards third parties such as airplane pilots.