What is paroxysmal tachycardia?
The term paroxysmal tachycardia refers to an intense heartbeat that the patient suddenly experiences and which, after a variable duration, ceases just as suddenly.
The definition therefore refers to a symptom; the arrhythmias that can determine it are many. Those that cause it most frequently originate from the atria and the electrical junction area between the atria and ventricles: they have a NON ventricular origin and are therefore defined as paroxysmal supraventricular tachycardias.
What is the danger of paroxysmal supraventricular arrhythmias?
In most cases these arrhythmias are not dangerous, also because they are not generally associated with structural heart disease. The patient feels a strong heartbeat and may be very bothered, but the heart's functioning remains sufficient to guarantee a valid circulatory function. If the arrhythmia occurs in patients with associated heart disease , then the impact on cardiac physiology may be greater and cause even significant symptoms.
What are the arrhythmias that most frequently cause paroxysmal supraventricular tachycardia?
The most frequent arrhythmia is paroxysmal nodal reentry tachycardia: it is characterized by an electrical short circuit that can be triggered between the two electrical conduction pathways located at the level of the electrical junction between the atria and ventricles. In most people, there is only one electrical pathway at this location that conducts the impulse from top to bottom. In a certain portion of the population, this electrical pathway can be split into two components, one with rapid conduction and one with slow conduction, and this constitutes the basis for triggering a short circuit that activates the heart at a high frequency (fig. 1).
What is paroxysmal reentrant tachycardia via anomalous pathway?
Another form of arrhythmia is paroxysmal reentry tachycardia through an anomalous pathway. In this case, the short circuit occurs between the atrioventricular junction and an accessory conduction pathway between the atria and ventricles, present from birth in a different part of the heart (fig. 2).
The electrical activation that reaches the ventricles through the atrioventricular node (Fig. 2 point A), instead of dying out to make room for the next cardiac cycle, returns back to the atria through the anomalous pathway (Fig. 2 point B) to then activate the ventricles again, causing an uninterrupted short circuit.
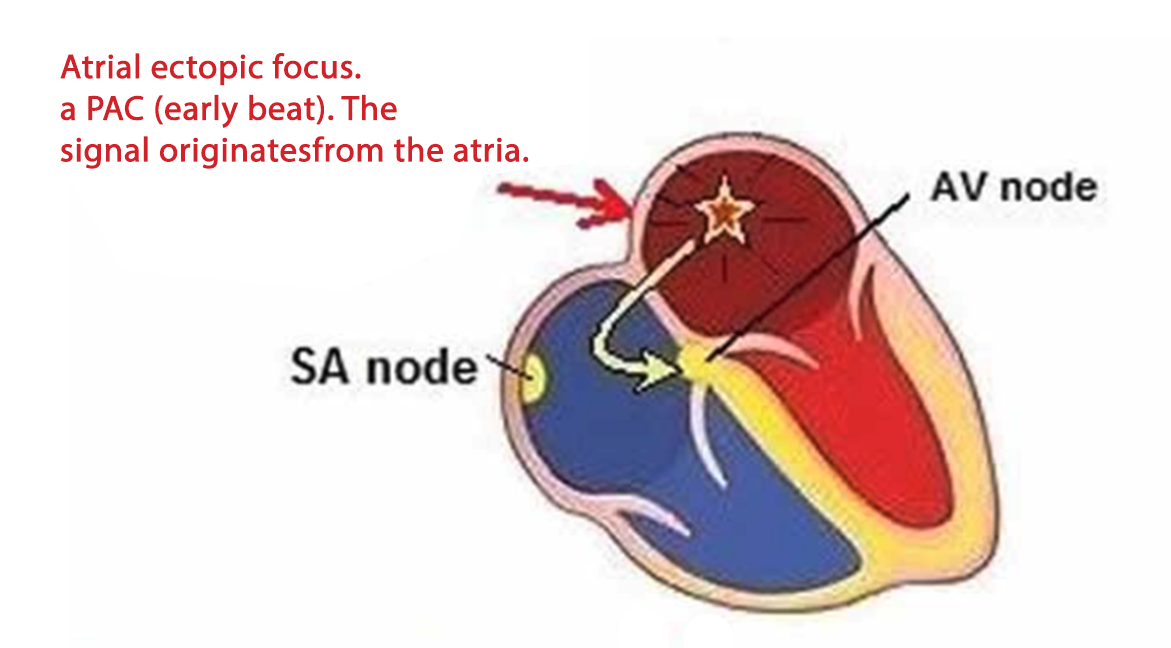
Atrial tachycardias
There are also other forms of paroxysmal tachycardia supported by arrhythmias that are localized in the atria, atrial tachycardias. They occur due to a short circuit localized inside the atrial cavities or due to the presence of a focus that activates extremely rapidly like a light bulb that switches on and off rapidly intermittently (fig. 3).
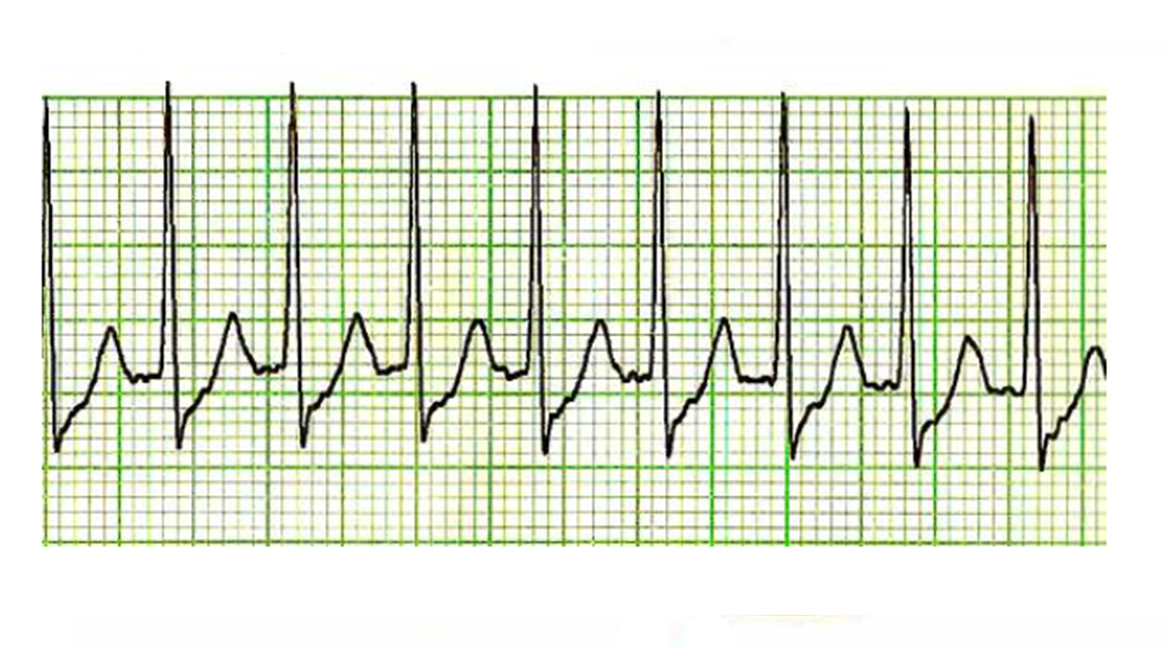
How is paroxysmal tachycardia diagnosed?
The diagnosis of paroxysmal tachycardia is made with the electrocardiogram which must be performed when the arrhythmia is in progress.
Performing an electrocardiogram when tachycardia is not in progress is generally not sufficient and only in some cases can it provide useful information, such as signaling the presence of WPW syndrome.
Once the diagnosis has been made, depending on the patient's clinical characteristics, tests are performed to evaluate the presence of associated clinical conditions such as a possible hyperthyroidism (blood test) or the presence of an associated heart disease (echocardiogram, coronary angiography, cardiac magnetic resonance imaging).
The electrocardiogram alone is almost never able to distinguish between the different mechanisms underlying paroxysmal supraventricular tachycardia. Therefore, for a complete diagnosis, an electrophysiological study is necessary.