Come nasce l’ablazione della fibrillazione atriale?
Atrial fibrillation is a widespread arrhythmia with a significant health impact. Medical therapies aimed at restoring a stable sinus rhythm often yield unsatisfactory results. There is a strong need for an effective cure for this rhythm disorder. Since the 1990s, researchers have sought methods to eliminate the cardiac cells and tissues in the atria that trigger and sustain atrial fibrillation. While early surgical methods were successful in maintaining sinus rhythm, the need for full cardiac surgery—and its potential complications—limited the expansion of this approach.
Thus, techniques were developed to remove diseased cells using catheters that reach the heart via blood vessels, avoiding surgery. This catheter ablation allows for treatment without surgical risks.
Who Should Undergo Atrial Fibrillation Ablation?
Patients with atrial fibrillation who do not respond to, cannot tolerate, or cannot take antiarrhythmic medications should undergo ablation. Ablation can also be performed as a first-line treatment for patients who prefer not to take long-term medication. However, it is not recommended for patients where restoring sinus rhythm is considered inappropriate due to advanced atrial disease, severe comorbidities, or advanced age.
How Is Atrial Fibrillation Ablation Performed?
The main goal of atrial fibrillation ablation is to eliminate cells that trigger and sustain the arrhythmia. These cells are located in the left atrium, and in the early stages of atrial fibrillation, they are predominantly found around the pulmonary vein openings. In such cases, ablation involves isolating the electrical activity in this area, creating what is called pulmonary vein disconnection or isolation (Fig. 1).
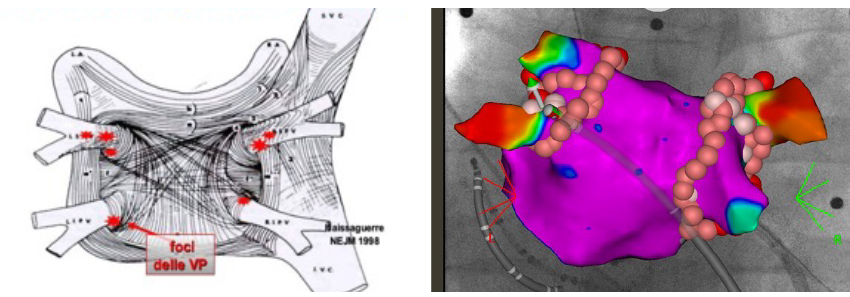
B: Pulmonary vein disconnection is achieved by creating ablative lesions, electrically isolating these foci so they no longer transmit arrhythmia to the atrium.
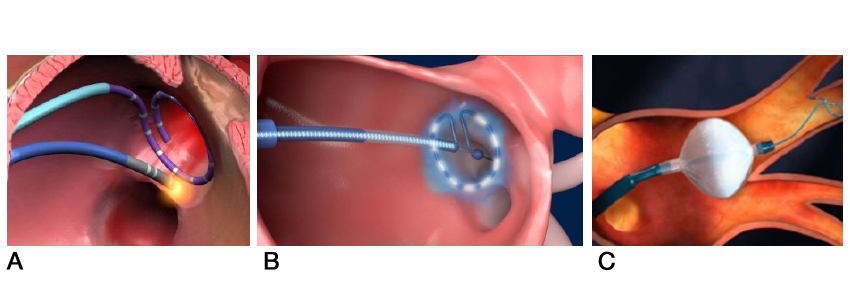
Complete isolation of the pulmonary veins can be achieved using various methods and energy sources, including radiofrequency, pulsed electrical energy, and cryoenergy. Catheters are advanced through the femoral veins, and after crossing the septum dividing the two atria, ablation is performed.
as the disease progresses, cellular alterations spread throughout a significant portion of the atrium. This necessitates extending the ablation to larger areas by creating linear ablation lines, which prevent the propagation of pathological short circuits (linear ablation).
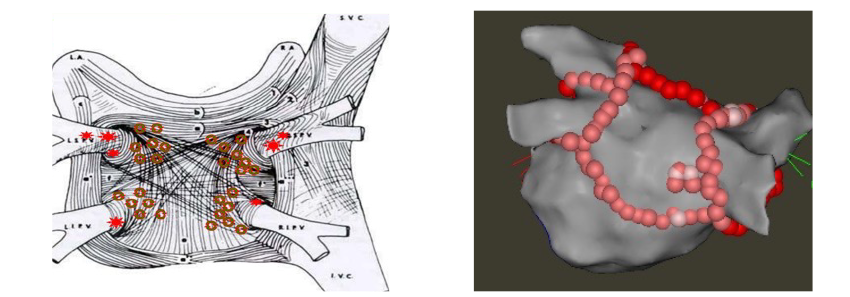
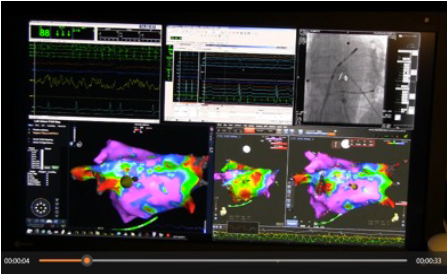
In questi casi assume molta importanza l’utilizzo di sistemi di mappaggio elettrico ed anatomico della cavità atriale che consente di identificare con estrema accuratezza le aree di tessuto atriale alterato e guidare con precisione il catetere ablatore evitando del tutto o quasi l’utilizzo dei raggi X (procedure a raggi zero).
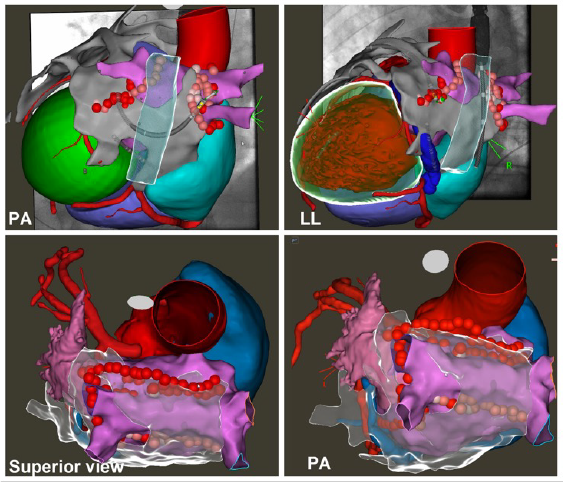
In advanced cases of atrial fibrillation resistant to transcatheter ablation, even with extensive linear lesions, Dr. Stefano Grossi has developed an endo-epicardial ablation technique combined with the exclusion of the left atrial appendage using the Lariat system (link). This approach, performed for the first time globally at the Mauriziano Hospital in Turin in 2022 (link articles), involves ablating both the internal and external heart surfaces. This creates full-thickness lesions capable of eliminating deeply located diseased cardiac muscle tissues that traditional techniques could not reach. The method has achieved highly satisfactory outcomes, with a stable restoration of sinus rhythm in over 90% of patients with particularly advanced atrial fibrillation.
Results of Atrial Fibrillation Ablation
Transcatheter ablation of atrial fibrillation maintains stable sinus rhythm in 70-80% of patients with paroxysmal atrial fibrillation (less severe form) and 60-70% of those with persistent forms (more advanced cases).
These results significantly reduce patient mortality, hospitalization rates, incidence of stroke, dementia, and improve physical and mental functional states, as well as overall quality of life.
In patients with associated heart disease and heart failure, the impact on reducing mortality and hospitalization rates is even greater. These patients derive the most significant clinical benefit.
Anticoagulant Therapy and Ablation
Before undergoing atrial fibrillation ablation, patients must take oral anticoagulant therapy for at least one month to prevent blood clots from forming in the atrial cavity during the procedure.
Upon hospital admission, a transesophageal echocardiogram is performed to definitively exclude the presence of clots. The close proximity between the esophagus and heart allows excellent visualization of the atrial cavities.
Anticoagulant therapy is not discontinued for the ablation procedure and is continued for three months afterward. During a follow-up arrhythmology consultation, the physician will decide whether to continue anticoagulation based on the patient's thromboembolic risk.
Is Ablation Performed Under Anesthesia?
For many years, Dr. Stefano Grossi has been among the first in Italy to perform atrial fibrillation ablation procedures under deep sedation. To date, he has handled over 5,000 cases.
This is not full anesthesia. The patient breathes spontaneously without intubation but is deeply sedated, feeling no pain or anxiety during the procedure.
Once the sedative is stopped, the patient quickly regains consciousness and is transferred to the recovery ward within minutes.
Post-Ablation Recovery
Recovery after atrial fibrillation ablation is rapid. The patient remains in bed for 8 hours, and after clinical and echocardiographic evaluations, they are discharged the following day.
For several days, the patient should lead a tranquil life, avoiding exertion and physical activity.
Approximately three months later, Dr. Grossi recommends a follow-up arrhythmology consultation, preceded by a 24-hour ECG Holter test.